Frequently Asked Questions
MOST FREQUENT QUESTION - GENERALWhat is Thalassemia?
Thalassemia is a genetic or an inherited disorder of the blood. It is not a disease. In this disorder, body is unable to produce adequate amount of red pigment of blood commonly called as Hemoglobin (Hb). The size of the red blood cells is smaller and the longevity of the red blood cells is reduced due to defective hemoglobin. This results in severely anemic condition which can lead to reduced life and even death.
Is Thalassemia known by any other name?
Thalassemia is also known as “Colley’s Anemia” and “Mediterranean Anemia”.
What are different types of Thalassemia?
Thalassemia is essentially of three types: Thalassemia Minor, Thalassemia Major, and Thalassemia Intermedia.
- Thalassemia Minor. Also known as Thalassemia Trait and Thalassemia Carrier. Those having this disorders have no apparent symptoms or illness, individuals appear perfectly normal and the disorder is discovered only when the person’s blood is tested for the same. The person having Thalassemia Trait are carriers of Thalassemia and can pass this disorder to the next generation. If one Thalassemic trait marries another Thalassemic trait, then there are 25% chances with every pregnancy, that the child will have thalassemia major. This disorder is described next.
- Thalassemia Major. This is a serious condition that requires to be managed clinically if the person is to lead normal life. The person requires blood transfusion at regular interval throughout his/her life. Some other medications and medical tests are also needed to monitor the well-being of the person.
Thalassemia Intermedia. It is a clinical condition of intermediate severity between major and minor Thalassemia. The condition usually manifests itself between four and eight years of age. Its management varies depending on the severity of the disorder.
How is Thalassemia transmitted from parents to their children?
Thalassemia is transmitted by the parents to the children. Thalassemia cannot occur if none of the parents is a Thalassemia carrier. If only one parent is Thalassemia carrier, then there are 50% chances that each of the children will also have Thalassemia Minor. If both parents are Thalassemia minor and a conception occurs, then there are only 25% chances that the child will be free of Thalassemia, 50% chances that the child will have Thalassemia minor and 25% chances that the child will have Thalassemia Major. These possibilities are in each conception. Thus, there is a possibility that all the children may have Thalassemia Major, or Thalassemia minor or be totally healthy. If one of the parents is Thalassemia Major, then all the children will be born with Thalassemia minor. (See Illustration)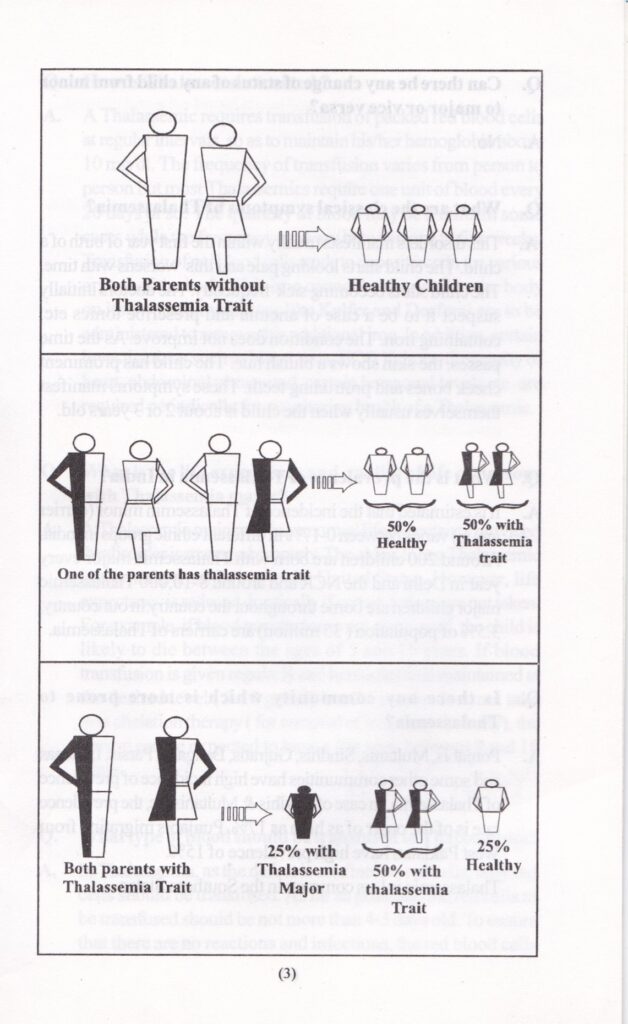
Can Thalassemia be acquired after birth?
No
Can there be any change of status of any child from minor to major or vice versa?
No
What are the classical symptoms of Thalassemia?
This order usually manifests within the first year of birth of a child. The child starts looking pale and this worsens with time. The child starts becoming sick frequently. The doctors initially suspect it to be case of anemia and prescribes tonics etc. containing iron. The condition does not improve. As the time passes, the skin shows a bluish hue. These symptoms manifest themselves when the child is about 2-3 years old. As the child grows, other deformities like elongation of jaw and protruding teeth may also take place.
What is the prevalence of Thalassemia in India?
It is estimated that the incidence of Thalassemia minor (carrier group) varies between 0-17% in different ethnic groups in India. Around 200 children are born with Thalassemia major every year in Delhi and the NCR. Approximately, 8-12,000 Thalassemia major children are born throughout India every year. In India, 3.5-4% of population are carrier of Thalassemia.
Is there any community that is more prone to Thalassemia?
Punjabis, Multanis, Gujratis, Sinhis, Parsis, Lohanas and some other communities have high incidence of prevalence of Thalassemia. In case of Sindhis and Multanis etc. the prevalence rate is of the order of as high as 17-18%. Punjabis who migrated from West Pakistan have high prevalence of 15%. Thalassemia is less common in the South Indian states.
How is Thalassemia treated?
Thalassemia requires transfusion of packed red blood cells at regular interval, so as to maintain his/her hemoglobin above 10 mg/dl. The frequency varies from person to person but most Thalassemics require one unit of blood every 20 days or so. The quantity of blood may be two units in some cases while the frequency can vary between one to five weeks. Transfusion of red blood cells tends to deposit iron in various organs of the body. This iron cannot be excreted by the body on its own and medicines like Kelfer, Desfral, Asunra, Desirox etc are to be administered to remove this additional iron. In addition, certain investigations such as blood tests, ECG, Echocardiography of the heart, abdominal ultrasound, MRI T2*, certain harmonal levels etc. are required periodically for monitoring health of a Thalassemic.
What is the life expectancy and quality of life of persons with Thalassemia major?
Thalassemia major can have normal life expectancy provided the disorder is managed properly. There are many Thalassemics who are grandparents today. However, life expectancy is reduced drastically if certain actions are not taken. For example, if blood transfusion is not given at all, the child is likely to die between the ages of 5 to 15 years. If blood transfusion is given regularly and hemoglobin is maintained at the desired level (9-10 gm/dl) but the person does not take iron chelation therapy (for removal of iron from the body), the person can be expected to have a life span of 8 to 18 years. With advances in medicine, life expectancy of the Thalassemics is increasing every decade.
What type of blood should be transfused to Thalassemics?
In Thalassemia, as the defect is confined to red cells, only red cells should be transfused. As far as possible, the red cells to be transfused should be not more than 4-5 days old. To ensure there is no reaction and infections, red blood cells should be filtered and it should be ensured that the packed red blood cells are totally free of white blood cells and plasma. As far as possible, the blood should be Nac tested to minimize infection from other sources.
Why is Leuko-reduction of blood necessary?
Leukocytes or white blood cells in blood are responsible for some harmful effects/reactions associated with blood transfusion. Some of these are:
- Fever reaction during/within 24 hours of transfusion.
- Transmission of certain viral infectious agents residing in white blood cells.
- Suppression of immune systems of the individual.
- Formation of antibodies in the recipient making him/her vulnerable to some diseases.
What are the various types of 'Leukoreduction'?
Filtration of blood can be done at three points:
- Fever reaction during/within 24 hours of transfusion.
- Transmission of certain viral infectious agents residing in white blood cells.
- Suppression of immune systems of the individual.
- Formation of antibodies in the recipient making him/her vulnerable to some diseases.
- At bedside when packed red blood cells are being transfused. The type of filter would decide the degree of filtration. However, some white blood cells tend to get dissolved and cannot be removed by the filter.
- Leukoreduction or filtration at the moment of issue of blood from the blood bank. This method has similar disadvantages as in case of bedside filtration.
- Pre-storage leukoreduction. In this case, the red blood cells are filtered immediately or within six hours of collection after the donor donates the blood. This method ensures that between 99 and 99.99% of white blood cells are filtered out thus ensuring there are practically no adverse effects on the recipients.
What iron chelating drugs are available?
Presently, there are three categories of medicines are available for iron chelation. Desfral is administered by injection usually at night for 4-5 nights a week. Kelfer is administered orally and has to be taken every day. The latest medicines are of “Exjade” family of which Asunra and Desirox are the most common. There are other brands too belonging to the same family. All these medicines have some side effects but these are not very serious and with due care, these effects can be minimized.
Is Thalassemia preventable?
Yes. Thalassemia is an entirely avoidable condition. In fact, its prevention is much simpler than its treatment. The most important step in prevention of Thalassemia is detection of its carriers for which a simple blood test is required. Those having Thalassemia trait or Thalassemia major should avoid marriage with another Thalassemia minors. Even if the marriage between two Thalassemic carriers does take place, it can be ensured that the off springs do not have Thalassemia major. This is done by testing fetus and if found to be Thalassemia major, an abortion can be considered.
Can Thalassemia be cured?
The only way this disorder can be cured presently is by having Bone Marrow Transplantation or BMT. For better results, the bone marrow transplantation should be done at an early age. The problem is finding a perfect donor. Normally siblings are the ideal persons for this purpose. It must be remembered that the donor in this case carries no risk whatsoever. Since this is a genetic disorder, other alternative treatment is stem cell therapy. It is extremely expensive and the treatment is presently available only in the United States and some European countries.